Abigail:
It’s hard to believe that we’ve been in PNG for over a month already. In some ways, it feels like we have only been in Kudjip for a few days, and in other ways it feels like Kudjip has been our home for years.
We are feeling mostly settled in and are finding our daily rhythm at home and in the hospital. We have shared many meals with fellow missionaries and it has been lovely to learn about the people we are serving with. One of our favorite activities is going for an evening walk around the station and getting to chat with our new friends. There are 2 other families in Kudjip who are currently in the Post-Residency Program through Samaritan’s Purse (and many other families who are graduates of this program), and it has been a particular blessing to spend time learning from and with them (shout out to the Stewardson and Morris families). They have quickly become good friends of ours and we appreciate how they have taken us under their wings.

For our first two weeks in Kudjip, we spent our mornings unpacking, getting groceries, familiarizing ourselves with our new home, or working in the hospital. Our afternoons were spent doing language training with our language teachers, Moses and Lucy. They have taught us so much about the Pidgin language and about the culture of PNG. We have been blessed by their instruction, friendship, and patience with us as we (particularly me) made many mistakes when trying to speak Pidgin. Although our formal language training with Moses and Lucy is complete, they remain good friends and we enjoy how often we get to see Lucy since she works at the hospital.
Brian has been able to reconnect with many friends that he has previously made on his trips to PNG. When he was here in 2013, he worked with a crew of five local men. He’s reconnected with four of them and we’ve even hired one of them to help clear the land in our backyard that will become our garden. Other staff in the hospital have worked here for years and it’s wonderful to see familiar faces and know that we will get to work with them for years to come.
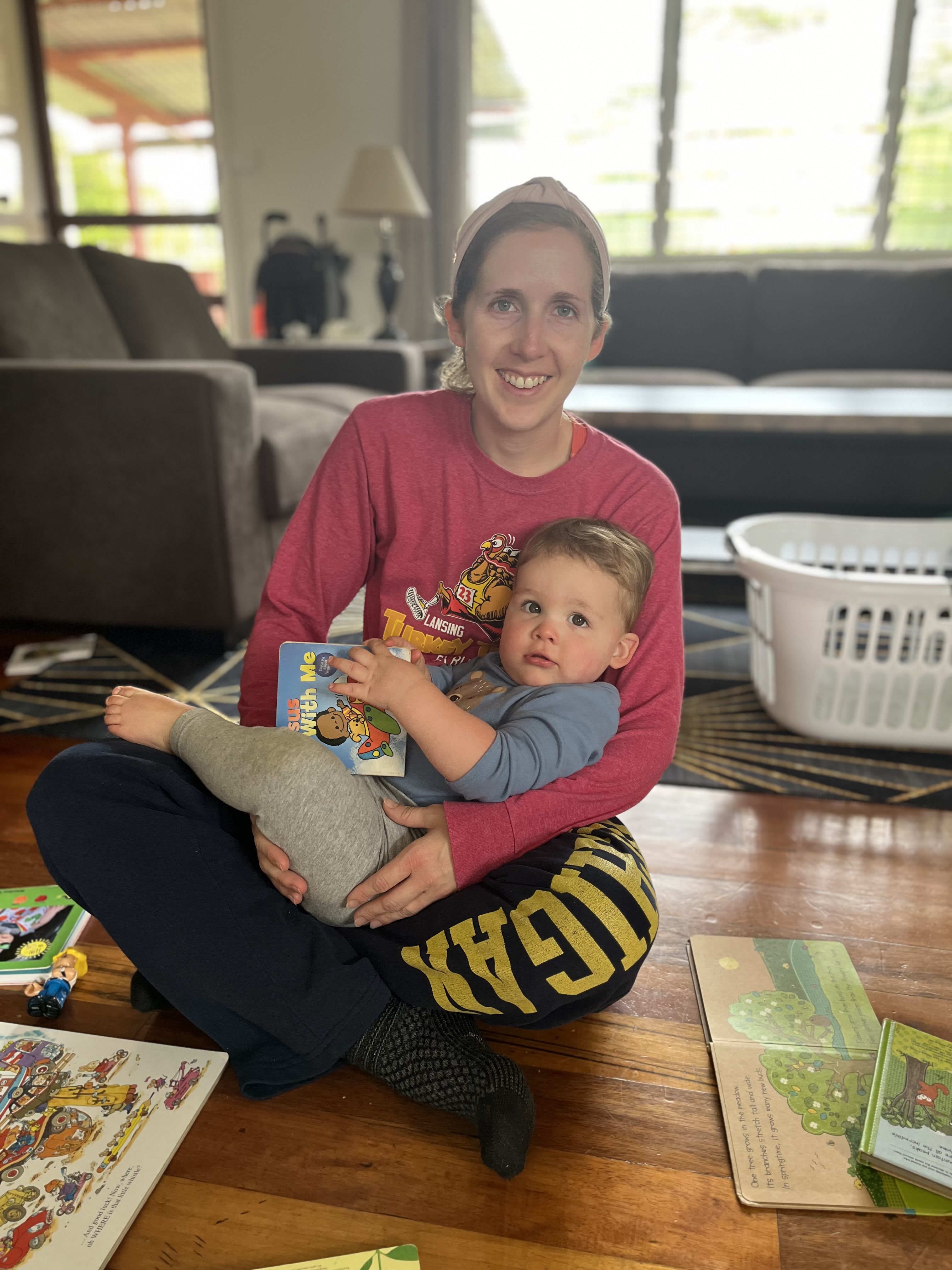
I have been caring for Henry at home and working to train the women who will be looking after Henry once she starts working in the hospital more. It has been both rewarding and challenging to be home full-time, and I am trying to find the right balance of responsibilities at the hospital with responsibilities at home. I have met with hospital leadership about how my medical expertise can best be utilized in the hospital and community. There are ample opportunities to care for pediatric patients at the hospital and opportunities to further develop palliative care services too. Having a two physician household means that we must both be flexible when it comes to our day-to-day schedules, especially as we navigate hiring nannies to care for Henry. I have really enjoyed getting to know the women who will be caring for Henry and they have helped her practice Pidgin. As we continue to figure things out, we are so grateful for colleagues who understand the complex needs of being parents and missionary doctors.

Brian:
Spoiled
In preparing to serve in a mission hospital, there were many feelings I anticipated: overwhelmed, in over my head, under-resourced. One feeling that I did not anticipate: spoiled. In many ways I honestly feel spoiled serving at Kudjip Nazarene Hospital. In the surgery department, I have excellent colleagues in the other surgeons, strong nursing and operating room teams (camaraderie is a big deal in stressful environments like the OR), a decent supply of instruments and equipment, fairly reliable internet and power, and experienced surgery trainees. All of these things make my transition to missionary medicine much easier and less stressful. While our hospital resources are not that of even small US hospitals, we have more diagnostic and operating equipment than I anticipated having and the general attitude of the hospital is much more resourceful and less wasteful. I recently talked with a doctor from New Zealand who serves at very remote hospitals in PNG that are staffed by 1-2 physicians at a time. She said that some of these hospitals often do not have simple things like gauze and bandages in stock. That really puts into perspective our relative abundance of resources. We often make light of the resources we do NOT have: CT scan, interventional radiology, an ICU, etc. but I always have tools and a trained team to assist me, which is more than can be said for many places in this country.

My first month in the hospital has been a ton of learning. I’ve done a lot of procedures that I feel very comfortable with: appendectomies, hernia repairs, intestinal resections, abscess drainage. I’m also learning to be comfortable with other things that were previously outside of my wheelhouse: C-sections, tubal ligations, drainage of tubo-ovarian abscess, hysterectomy, ruptured ectopic pregnancies (note these are all OBGYN, so still in the abdomen/pelvis and thus not too terribly foreign to me). And still there are other things that I’ve never done before in my life: hemiglossectomy (removal of part of the tongue), lots of orthopedic procedures (tendon repairs, bone plating for fractures, and foot repair with wires so far), lateral canthotomy (an ophthalmology procedure), and peritonsillar abscess drainage. Learning in the OR is fun. Plus we get to see patients get better in most cases, which is rewarding.
In my medical training, I’ve unfortunately gained plenty of experience in breaking bad news. This often came in the form of revealing cancer diagnoses, telling a family about their loved one’s death, and discussing mortality and bleak outlooks with patients and families. This is a heavy responsibility and always emotionally taxing. Here in PNG, the demands are so high that somedays this emotional toll can feel overwhelming. On my first independent clinic day, a surgery trainee and I saw over 30 new consults. At least 9 of these were new cancer diagnoses, most of which were metastatic and thus not curable. Discussing this heavy news with patients time after time, while knowing that the waiting room is full with patients waiting to be seen, made for the most exhausting day for me thus far. It makes me frustrated that I cannot help everyone and that so many cancers here present late when surgical resection is no longer possible. But it does cause me to take a step back and gain perspective: even if I were able to save these people from cancer, I wouldn’t be able to extend their lives forever. This underlines the crux of our work here: We treat, Jesus heals. These tough conversations with patients often start with an admission that I cannot cure their physical illness and that we all will die someday, but in Jesus we all can live eternally.
An example of this is a patient I saw in clinic who complained of weight loss, inability to eat, and abdominal pain and distention. Based on this and his physical exam, I was concerned for a near-obstructing cancer somewhere in the GI tract. He was admitted to the hospital and I performed abdominal exploration to find a massive stomach tumor that obstructed the outflow of the stomach and was invading the blood vessels of the liver with palpable lymph nodes everywhere – totally unresectable. I performed a palliative bypass to allow the stomach to drain which will allow him to eat after he heals. A couple of days after his procedure as he was recovering in the hospital I sat down and discussed my findings and the fact that this cancer would kill him. He told me that he had been a church-going man previously, but had strayed in recent years. This illness had brought his focus back to God. I prayed with him and reminded him that “taim long yumi stap long dispela graun em i sotpela tru, tasol wantaim Jisas, yumi bai stap long ples heven oltaim oltaim” (Our time on this Earth is very short, but through Christ, we will live in Heaven forever). We treat, Jesus heals.

Support
In preparing to leave for PNG, we spoke at several churches and sent out letters requesting support from family and friends. We have been blown away by the generosity we have received. It’s truly humbling to have people giving financially and to receive emails from people reminding us that they are praying for us and our work. To all of the partners we say thank you.
Just a few examples of what your financial support goes toward:
- Brian flying to Australia to take his general surgery board exam
- car trips into town to buy groceries
- excess baggage fees as we moved our lives across the ocean
- hiring childcare for Henry
Praises and requests:
- we have found two wonderful ladies who watch Henry for 3 full days each week. This allows both of us to work in the hospital these days. Having these trusted women with whom we get to build relationships is great (plus Henry already loves them).
- Such a wonderful community and many new friends who have been intentional about checking in on us and answering our many many questions
- This next Wednesday, we will fly on a small Missions Aviation Fellowship plane to Kompiam, a smaller rural hospital, where we will undergo 2 weeks of language and cultural training. Please pray for safety in travels and adjustment in a new place.
- Continue to pray for us as we learn. Learning not only entails broadening our medical scope of practice, but adapting to different and limited resources and different pathologies in a different language and culture. This is not just in the hospital, but at home and in the larger community as well.
- Continue to pray for our patients and those we are called here to serve. There is a lot of suffering in the world, from both natural and manmade causes, and we hope to share Christ’s light in this darkness.








Leave a reply to Mark & Bonnie Cancel reply